GM case discussions on Kidney Failure
CASE 1:
The complete case can be viewed here:
https://alekyatummala.blogspot.com/2020/09/45-yr-female-with-anasarca.html?m=1
A 45 year old female came to the OPD with chief complaints of:
• Pedal edema- pitting type , which is progressive and later developed abdominal distension and facial edema.
• Also associated with decreased urine output, shortness of breath ( even at rest ) , right sided chest pain- non radiating and associated with palpitations.
• No h/o fever, burning micturition, hematuria or frothy urine.


HOPI:
• Patient was apparently asymptomatic 6 months ago, when she started developing episodes of pedal edema which used to increase on walking and decrease on rest.
• This was also associated with grade 3 dyspnea
• She was advises fluid restriction for her edema
• Since the past five days, she started developing the present symptoms.
PAST HISTORY:
The patient is a known case of:
• Diabetes Mellitus Type 2 since the past 5 years.
• HTN since the past 1 year
No relevant family history
PERSONAL HISTORY:
• Diet mixed and appetite normal
• Sleep adequate
• Bowel and Bladder movements- reduced since 3 days.
• H/o tobacco chewing since 8 years
EXAMINATION:
Patient is conscious , coherent and cooperative
Pallor present. No signs of icterus, cyanosis, koilonychia, lymphadenopathy.
Ulcer on right sole.
VITALS:
• Temperature-afebrile
• BP- 180/80 mm hg
• Pulse- 84 bpm
• RR- 13 cycles/min
CNS- S1 S2 heard, no murmurs
RS- Bilateral air entry +
CNS-
Higher mental functions and Cranial nerves- intact.
Motor and sensory systems- normal.
No cerebellar or meningeal signs.
INVESTIGATIONS:

ABNORMAL RFT WITH RAISED UREA, CREATININE AND URIC ACID LEVELS

HEMOGRAM SHOWS MICROCYTIC HYPOCHROMIC ANEMIA

CUE IS POSITIVE FOR ALBUMIN INDICATING PROTEINURIA

ABG-INDICATED METABOLIC ACIDOSIS

ULTRASOUND- NORMAL

DAY3 -COLOUR DOPPLER 2D ECHO SHOWS DYASTOLIC DYSFUNCTION ALONG WITH MITRAL VALVE AND TRICUSPID VALVE DYSFUNCTION.

ON DAY 4 SHE DEVELOPED PLUERAL EFFUSION.
DAY 5- RENAL VEIN DOPPLER WAS DONE TO RULE OUT RENAL VEIN THROMBOSIS.
COURSE IN THE HOSPITAL:
DAY 1: Treated with bicarbonate for metabolic acidosis and was kept on OHA and antihypertensives
DAY 2: Developed pain abdomen and did not pass urine. No suprapubic tenderness or burning micturitio
DAY 3: Dialysis was done as there was refractory anuria. Ophthalmology examination showed moderate hypertensive retinopathy changes.
DAY 4: C/O abdominal pain with facial puffiness, abdominal distension and pedal edema. Dialysis with blood transfusion was done.
1) What is your complete anatomic and etiologic diagnosis from the data available in the patient's online record linked above? (ignore the provisional diagnosis on admission mentioned in the case report)
Kidney failure which may be secondary to diabetes and hypertension associated with anaemia which has progressed to heart failure with diastolic dysfunction. ( cardiorenal syndrome )
DIABETIC NEPHROPATHY:
Diabetic nephropathy is a significant cause of chronic kidney disease and end-stage renal failure globally.
DN is characterized by structural and functional changes. In glomeruli, there is mesangial expansion, thickening of the basement membrane, and, characteristically, nodular glomerulosclerosis (Kimmelstiel–Wilson nodules). In early DN, tubular hypertrophy is present but eventually interstitial fibrosis with tubular atrophy develops, along with arteriolar hyalinosis. In advanced cases, there is an infiltrate of macrophages and T-lymphocytes. Ultrastructurally, there is podocyte loss and reduced endothelial cell fenestration.These characteristic pathological changes are shown in . Functionally, there is early glomerular hyperfiltration and increased albumin excretion; and with advancing nephropathy, increasing proteinuria and declining GFR.

2) What are the reasons for her:
Azotemia:
Azotemia is a biochemical abnormality, defined as elevation, or buildup of nitrogenous products (BUN- usually ranging 7 to 21 mg/dl), creatinine in the blood, and other secondary waste products within the body.
Raising the level of nitrogenous waste is attributed to the inability of the renal system to filter ( decreased GFR) waste products adequately. It is a typical feature of both acute and chronic kidney injury.
Azotemia becomes manifested in a constellation of clinical signs and symptoms along with biochemical abnormalities; it is termed as uremia.
Anemia:
Kidneys make an important hormone called erythropoietin (EPO). EPO causes synthesis of red blood cells. In Chronic kidney failure, kidneys cannot produce enough erythropoietin which lead to decreased RBC production and anemia develops.
Hypoalbuminemia:
Hypoalbuminemia is common in end-stage kidney disease. It is causes by a combination of a reduced synthesis and an increased degradation of albumin. The altered albumin homeostasis is caused by a systemic inflammatory state.
Progressive kidney damage leads to proteinuria which further leads to albuminuria and hypoalbuminemia.
Acidosis:
Metabolic acidosis is one of the most common consequences of chronic kidney disease ( CKD ), and it’s prevalence increases with declining GFR. Kidney has a central role in maintaining bicarbonate homeostasis. In kidney diseases, impaired ammonia excretion, reduced tubular bicarbonate reabsorption and insufficient renal bicarbonate production in relation to acid synthesised by the body causes metabolic acidosis.
3) What was the rationale for her treatment plan detailed day wise in the record?
Particularly mention rationale and efficacy for some of the drugs administered such as oral and iv bicarbonate? When is iv or oral bicarbonate indicated and why is it contraindicated in certain situations?
Rationale for her day wise treatment plan:
DAY 1:
• inj NaHCO3 for metabolic acidosis
• syr Potchlor for treating hypokalemia
• oral hypoglycaemic agents and anti hypertensive for control diabetics and hypertension respectively.
DAY 2:
• inj HAI on sliding scale- human regular insulin for controlling blood sugar.
• tab orofer- ferrous ascorbate (iron) and folic acid (vit B9) supplement given to treat her anemia
• tab pantoprazole- antacid
• inj lasix- furosemide- loop diuretic to treat fluid retention and edema.
DAY 3:
• inj lasix
• inj HAI on sliding scale
• syr potchlor
• tab dytor- also a diuretic
• tab telma (telmesartan) - Angiotensin receptor blocker and tab nifedipine ( calcium Channel blocker) used to treat high blood pressure.
• Inj erythropoietin - to treat anemia
• tab nodosis- antacid
• tab- shelcal ct- calcium supplement.
DAY 5:
• syr lactulose- synthetic disaccharide used in constipation and to prevent liver complications.
• protein powder
• inj monocef - cephalosporin antibiotic.
*Rationale for bicarbonate therapy in CKD:
Intravenous Sodium Bicarbonate therapy increases plasma bicarbonate, buffers excess hydrogen ion concentration, raises blood pH and reverses the clinical manifestations of metabolic acidosis seen in kidney diseases.
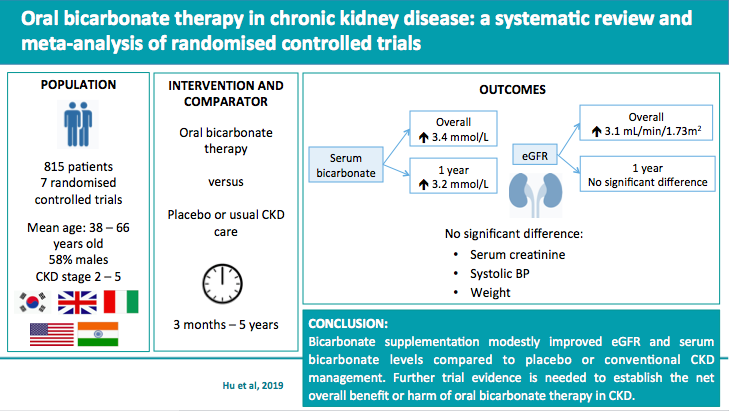
*Indications for bicarbonate therapy:
• severe metabolic acidosis which can occur in severe renal disease, uncontrolled diabetes, circulatory insufficiency due to shock, anoxia, severe dehydration, extracorporeal circulation of blood and severe primary lactic acidosis.
• tricyclic antidepressants, salicylate and phenobarbital overdose.
• hyperkalemia
• crush injuries
• hemolytic reactions requiring alkalinisation of urine to diminish nephrotoxicity of blood pigments.
*Contraindications for bicarbonate therapy:
• mentabolic and respiratory alkalosis
• in patients who are loosing chloride by vomitting or from continuous gastrointestinal suction or patients at risk of developing diuretic induced chloride loss to prevent hypochloremic acidosis.
• hypercarbic acidosis
• situations in where salt retention is undesirable- edema heart disease, cardiac decompensation, primary or secondary aldosteronism.
• in hypocalcemia as bicarbonate decreases ionised calcium in the serum and thus precipitates tetany.
•in hypokalemia as bicarbonate increases potassium uptake by muscle cells and thus further decreases serum potassium levels.
4) What was the indication for dialysing her and what was the crucial factor that led to the decision to dialyze her on the third day of admission?
Indications for Dialysis in a patient of CKD:
* Pericarditis and Pleuritis
* Progressive uraemia encephalopathy
* A clinically significant bleeding diathesis
* Hypertension is poorly responsive to antihypertensive drugs
* Fluid overload refractory to diuretics
* Metabolic disorders that are refractory to medical therapy such as hyperkalemia , hyponatremia, metabolic acidosis, hyper/hypo calcemia, and hyperphosphatemia.
* Persistant nausea and vomitting
* Evidence of malnutrition.
Ref:https://www.ncbi.nlm.nih.gov/books/NBK535404/
On the third day of admission, the patient was put on dialysis as she had Refractory Anuria and her BP was 170/90 inspite of being on antihypertensive drugs.
There was also Severe Shortness of Breath with Metabolic Acidosis.
5) What are the other factors other than diabetes and hypertension that led to her current condition?
Preciously used medications such as NSAIDs or ACE inhibitors which the patient might have used for hypertension could have caused a drug induced kidney damaged leading to her present condition.
Any previous infections could also play a part
6) What are the expected outcomes in this patient? Compare the outcomes of similar patients globally and share your summary with reference links.
"The major cause of morbidity and mortality in diabetes relates to cardiovascular complications. A person with diabetes has an annual mortality rate more than twice as high as a similar person without diabetes. The presence of early kidney disease roughly doubles the cardiovascular risk. Patients on dialysis have a mortality rate between 10 and 1000 times higher than age-matched controls. Patients attending a predialysis clinic are between two and 10 times more likely to die of a cardiovascular event than they are to require dialysis. It is important to recognize that people with diabetes and CKD are among those at highest risk for cardiovascular events.”
CKD in diabetes can be identified through routine laboratory testing, and this helps clinicians to identify people who are not only at risk of loss of kidney function, but those who are also at a significantly elevated cardiovascular risk."
Several decades of trials support the conclusion that cardiorenal risk in this population is modifiable and have contributed to the development of Canadian clinical practice guidelines in this area.
Clinicians should identify CKD in people with diabetes, as well as follow an aggressive, multifactorial approach aimed at reducing cardiorenal risk through lifestyle modification, control of glycemia, lipids and BP, use of acetylsalylic acid. ACE inhibitors and ARBs are strongly indicated in this polulation. Despite this aggressive approach, this population continues to be at a high risk of cardiovascular and renal events.
7) How and when would you evaluate her further for cardio renal HFpEF and what are the mechanisms of HFpEF in diabetic renal failure patients?
The cardiorenal syndrome (CRS) is a complex disease in which heart and kidney are simultaneously affected and their deleterious effects are reinforced in a feedback cycle, with accelerated progression of renal and myocardial damage.
Incidence of HFpEF increases with old age, diabetes, hypertension, obesity and CAD.
Patients usually presents with intermittent paroxysmal dyspnaea, orthopnea, dyspnea, fatigue, ascites and dependent edema.

Methods of evaluation:
| Diagnostic modality | Comment |
|---|---|
| ECG | Should be done yearly; for LVH and baseline rhythm |
| Resting echocardiography | LV function, RWMA, valvular disease; operator dependent |
| Cardiac SPECT | Variable sensitivity; effect of antihypertensive agents; good negative predictive value |
| Dobutamine stress echocardiography | More specific than SPECT for CAD; LVH is confounder; exercise intolerance |
| Stress CMR | Good sensitivity and specificity; not in eGFR <30 mL/min/m2 |
| Coronary CT angiography | Not in established CAD/ESRD; higher burden of coronary calcium confounder |
| Coronary angiography | Gold standard; invasive, loss of residual renal function |
8) What are the efficacies over placebo for the available therapeutic options being provided to her for her anemia?

The patient was given the following meditations for correcting anemia
• tab. Orofer BD
• inj erythropoietin (s/c) twice weekly
* packed red blood cell transfusion
* Efficacy of inj. Erythropoietin over placebo:
"The use of recombinant human erythropoietin in the correction of anemia in predialysis patients and its effect on renal function: a double-blind, placebo-controlled trial
Fourteen nondialyzed patients with chronic renal insufficiency (serum creatinine 265 to 972 μmol/L [3.0 to 11.0 mg/dL]) and severe anemia (hematocrit < 30%) were randomized to receive either recombinant human erythropoietin (r-HuEPO) or a placebo subcutaneously thrice weekly for 12 weeks or until reaching a hematocrit of 38% to 40%. Anemia was significantly ameliorated in the treated patients. No acceleration in the progression of renal failure (1/serum creatinine v time) or change in serum potassium was noted for either the placebo or treated group over the 12-week period. Six of seven treated patients had a significant decrease in serum ferritin and percent transferrin saturation (plasma iron/total iron-binding capacity). This resulted in functional iron deficiency and the requirement for iron supplementation. The average systolic and diastolic blood pressure did not differ significantly between the two groups of patients during the study. Quality of life was improved in all r-HuEPO-treated patients but not in those in the placebo group. This study demonstrates the safety and efficacy of r-HuEPO in the correction of anemia in predialysis patients without adverse effects on renal function over a 12-week period. Improved patient well-being as a result of the correction of anemia resulted in one patient refusing appropriate initiation of dialysis therapy.”
Ref:https://www.sciencedirect.com/science/article/pii/S0272638689801490
9) What is the utility of tools like the CKD-AQ that assess the frequency, severity, and impact on daily activities of symptoms of anemia of CKD? Is Telegu among the 68 languages in which it is translated?
The CKD-AQ, CHRONIC KIDNEY DISEASE- ANAEMIA QUESTIONNAIRE is a novel PRO measure that captures the frequency and severity of the most relevant symptoms and impacts associated with anaemia of CKD. Future studies will evaluate its psychometric properties and its potential utility in anaemia management.
The CKD-AQ contains 23 items covering relevant impacts and symptoms associated with anaemia in CKD.The measure was translated into 68 languages to facilitate its global clinical trials. The questionnaire contains 8 items that assess the frequency of each symptom, all rated on a 5-point verbal rating scale . An additional 8 items assess the severity of these symptoms using a 11-point numerical rating scale. Five items assess the ability to do various activities, and 2 items assess the emotional impact of anaemia of CKD.
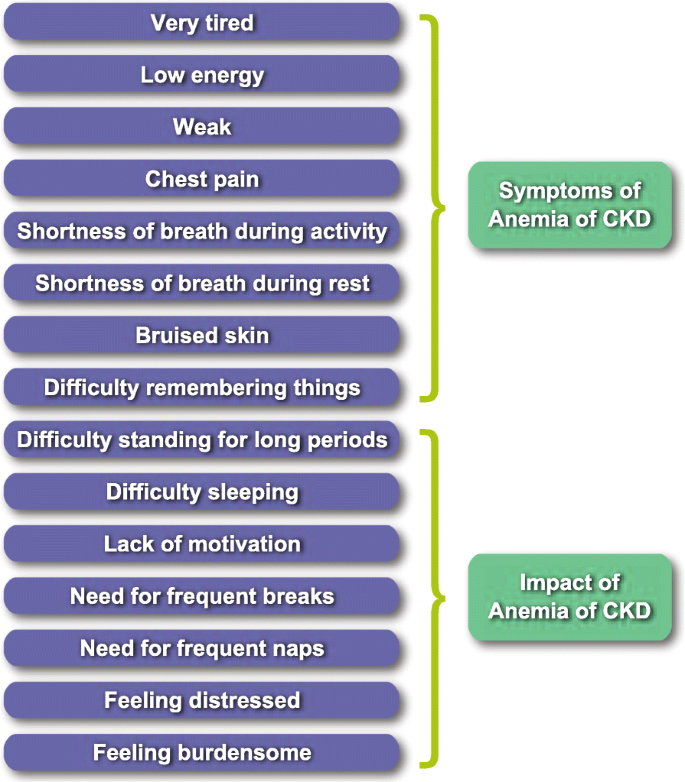
ref:Symptoms and impacts in anemia of chronic kidney disease ...jpro.springeropen.com › articles
10) What is the contribution of protein energy malnutrition to her severe hypoalbuminemia? What is the utility of tools such as SGA subjective global assessment in the evaluation of malnutrition in CRF patients?
Elevated protein catabolism and protein malnutrition are common in patients will chronic kidney disease (CKD) and end stage renal disease (ESRD). The underlying ethology includes, but is not limited to, metabolic acidosis, intestinal dysbiosis, systemic inflammation with activation of compliments, endothelia-1 and renin-angiotensin-aldosterone (RAAS) axis; anabolic hormone resistance; energy expenditure elevation; ureamic toxin accumulation.
Hypoalbuminemia in CKD-
"The factors regulating serum albumin are similar between individuals with and without CKD. Reduction in the glomerular filtration rate does not, in and of it- self, predispose to hypoalbuminemia. Individuals with hypoalbuminemia and advanced CKD have plasma albumin half-lives and degradation rates similar to those of healthy individualsand possibly even higher rates of albumin synthesis. Dialysis patients also show similar rates of albumin synthesis and turnover. However, conditions that often accompany CKD profoundly influence albumin synthesis. Among these are chronic metabolic acidosis and inflammation from concurrent illnesses. Therefore, apart from very rare circumstance in which dietary protein intake is minimal, hypoalbuminemia in CKD is driven primarily by nondietary factors."
Nutritional assessment of patients with chronic kidney disease is a vital function of healthcare providers. Subjective Global Assessment (SGA) is a tool that uses 5 components of medical history--weight change, dietary intake, gastrointestinal symptoms, functional capacity, disease and its relation to nutritional requirements and three components of brief physical examination science of fat and muscle eating, nutrition- associated alterations in fluid balance to assess nutritional status. SGA was originally used to predict outcomes in surgical patients; however, its use has gone beyond this function and population. In CKD,SGA is incorporated into the complete nutritional assessment. SGA has been altered by different researches and clinicians to better meet the needs of the patients they served. Further work in establishing validity and reliability of each version of SGA in different patient population should be done to enable clinicians and researchers to properly use this nutritional assessment tool.
CASE 2:
The complete case can be viewed here:
https://bhavyayammanuru.blogspot.com/2020/09/aki-secondary-to-uti.html?m=1
A 58 year old male came to the OPD with chief complaints of:
decreased urine output since 3 days
not passing urine since 1 day
pain abdomen since 1 day
HOPI:
patient was apparently asymptomatic 4 days back when he developed non productive cough, fever- low grade, continuous, not associated with chills and rigor. he then developed dribbling or urine and decreased urinary output associated with burning micturition.
PAST HISTORY:
known was of diabetes since 5 yrs and HTN since 8 months
PERSONAL HISTORY- occasional alcoholic.
ON EXAMINATION:
Pt was conscious , coherent and cooperative
No signs of pallor, icterus , cyanosis, koilonychia, lymphadenopathy
INVESTIGATIONS:

HEMOGRAM-NORMAL

INCREASED SERUM SODIUM LEVELS

HIGH FASTING RBS-POOR GLYCEMIC CONTROL

UREA AND SERUM CREATININE - RAISED
GLYCATED HEMOGLOBIN- 6.8%

ON IMAGING- bladder was slightly distended which may point to the possible post renal cause of AKI such as any obstruction.

ON USG- Asymmetrical kidneys with slightly shrunken lower kidney.
PROVISIONAL DIAGNOSIS OF PRE RENAL AKI WAS MADE.
TREATMENT:
Inj.Piptaz 2.5mg/IV/TID
Inj.Pantop 40mgIV OD
Inj.Lasix 40mg IV BD
Inj.HAI S/C according to sliding scale
Please comment on the differences in the diagnosis, therapy and outcomes in both these two patients.
The first case was a case of chronic kidney disease secondary to diabetes or hypertension where as the second case is case of Acute kidney disease due to pre renal cause or a post renal cause.
In the first case the therapy is mainly directed towards controlling her diabetes and hypertension and preventing fluid overload and metabolic acidosis and correcting anaemia whereas in the second case targeted therapy like antibiotics for controlling any septic states ( pre renal ) or relieving any obstruction ( post renal ) should be done.
In the first case the outcome might be poorer due to prolonged course of the disease might lead to multi organ damage whereas in the second case the outcome will be better if treated appropriately.
Would you agree with the provisional diagnosis shared for this 58 M in the online case report linked above?
The provisional diagnosis for the case is given as Pre Renal AKI with underlying diabetes and HTN.
Symptoms such as fever, burning micturition and an increased neutrophil count point to a possible state of sepsis which further led to Acute Renal Failure ( PRE RENAL AKI )
But on imaging, there was slight distention of bladder which is usually seen in POST RENAL AKI which is usually due to obstruction in the urinary start.

What are the findings in the ultrasound of both kidneys? How do you explain those findings? Would it explain the etiology for his renal failure?
On ultrasound, both the kidneys are asymmetrical:
RT KIDNEY- 10.2 X 4.7 cm
LEFT KIDNEY- 7.6 X 3.6 cm- size slightly reduced.
Shrunken kidneys are usually seen in severe acute infections of the kidney or when the kidneys are subjected low perfusion as in case of renal artery stenosis.
shrunken kidney can also occur in chronic kidney disease, in this case, which could have been due to underlying diabetes or hypertension or any drug insults.


Comments
Post a Comment