GM case discussion: Ascites
The entire cases for this topic can be found in the link given below.





•Hemogram: hb-9.6 g/dl, tlc-6700,pcv-28.6, plt-4.38

Pleural fluid analysis : exudative



ASCITES :
It is the accumulation of free fluid in the peritoneal cavity.
Small amounts are asymptomatic.
Lager accumulations (>1L) show:
• abdominal distension
• fullness of flanks
• shifting dullness on persuasion
• fluid thrill/fluid wave
• superficial abdominal veins if it is due to portal hypertension.
Depending up Serum Ascites Albumin gradient (SAAG) the causes of ascites can be divided into:
1. LOW SAAG ( EXUDATIVE )
- Malignant disease: hepatic, peritoneal
- Acute pancreatitis
- Lymphatic obstruction
- Infection: tuberculosis
- Nephrotic syndrome
- Hypothyroidism
2. HIGH SAAG ( TRANSUDATIVE )
- Cardiac failure
- Hepatic cirrhosis
- Hypoproteinemia: protein losing enteropathy, malnutrition
- Hepatic venous congestion: Budd-chiari, Sinusoidal syndrome
- Meig's syndrome
- Constrictive pericarditis
CASE 1:
A 55 yr old female patient came to the OPD with complaints of
• abdominal distension since 10 days
HOPI
• insidious development of dull aching type pain in the epigastrium and left hypochondrium, which relieved on self induced vomiting 2 years ago.
It increased of food intake and reduced on self induced vomiting.
• assc with weight loss and chronic fatigue
• she had one episode of blood vomiting (hematemesis)
• complaints of excessive night sweats.
• low grade fever with chills and cough presently.
No h/o bilious vomiting, melena, loose stools, constipation.
No significant past medical or family history.
EXAMINATION:
Patient conscious, coherent, cooperative
Temp-afebrile
Pulse-74 bpm
BP- 140/80 mm hg
RR-18 cycles/min
CVS RR CNS - normal on examination
P/A-
•abdomen distended
•abdominal girth- 85 cm
• linea nigra present
• Superficial engorged veins
• Tenderness over epigastrium and left hypochrondrium
• palpable mass in left hypochondrium- spleenomegaly
( 16 cm )
• shifting dullness and flank fullness present
• bowel sounds- heard

INVESTIGATIONS:
- Hemogram- microcytic hypochromic anemia
- LFT- increased total and direct bilirubin
Increased alkaline phosphatase levels
- Viral serology- negative for anti HAV antibodies, HbSAg, HIV
- ECG
- X Ray chest


- USG findings

* portal vein thrombosis
* moderate splenomegaly
* gross ascites
* anterior abdominal wall collaterals
- HRCT:
* Moderate splenomagaly
* Caudate lobe hypertrophy
* Left lobe little shrunken
*Abdominal collaterals
* Dilated portal vein
* Peripancreatic fat stranding



• Ascitic fluid tap- increased sugar and decreased LDH
• UPPER GI ENDOSCOPY:
Grade 4 oesophageal varices
DIAGNOSIS:
PORTAL HYPERTENSION ( may be secondary to liver cirrhosis) causing
• moderate splenomegaly ( due to increased spleenic vein pressure)
• grade 4 oesophageal varices
• gross ascites
• anterior abdominal wall collaterals
TREATMENT:
• tab lactulose
• tab carvedalol
• tab norflox
• tab pantop
• tab nuerobion forte
• tab orofer Po
• tab folate
• syrup zincovit
• salt and fluid restriction
• anticoagulant therapy
• oesophageal varices band ligation
• Porto systemic shunt surgery.
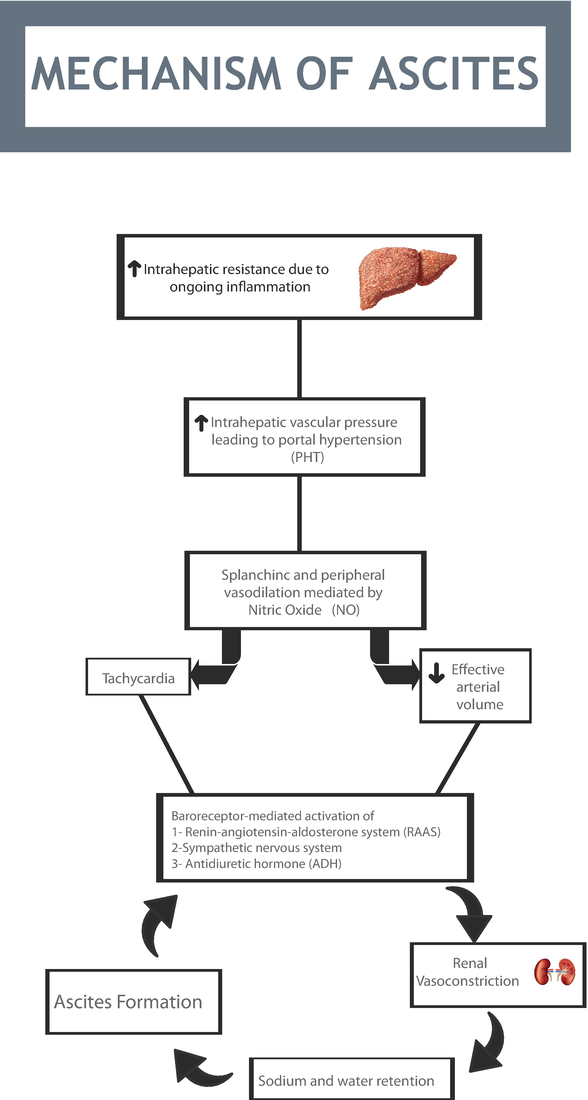
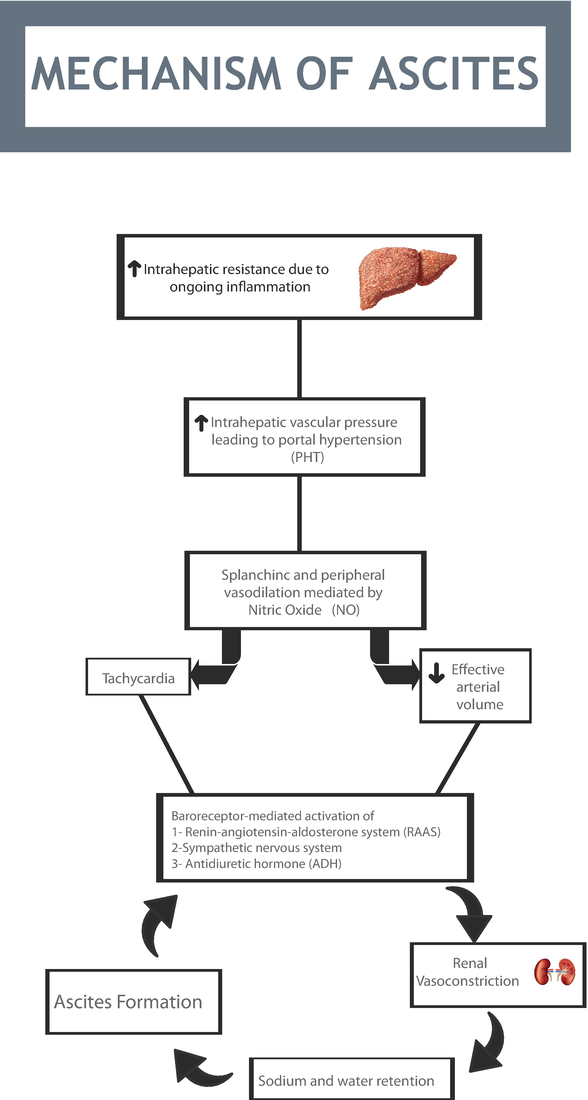
PORTAL HYPERTENSION:
Portal hypertension is an increase in the blood pressure within a system of veins called the portal venous system. Veins coming from the stomach, intestine, spleen, and pancreas merge into the portal vein, which then branches into smaller vessels and travels through the liver. If the vessels in the liver are blocked due to liver damage, blood cannot flow properly through the liver. As a result, high pressure in the portal system develops. This increased pressure in the portal vein may lead to the development of large, swollen veins (varices) within the esophagus, stomach, rectum, or umbilical area (belly button). Varices can rupture and bleed, resulting in potentially life-threatening complications.
The most common cause is cirrhosis of liver caused by hepatitis, alcohol, other less common causes of liver damage.
Other causes include:
- blood clots in portal vein
- blockage of veins that carry blood from liver to heart
- schistosomiasis
- focal nodular hyperplasia
- idiopathic
Clinical features:
- GI Bleeding marked by black, tarry stools or blood in the stools, or vomiting of blood due to the spontaneous rupture and hemorrhage from varices
- Ascites (an accumulation of fluid in the abdomen)
- Encephalopathy or confusion and forgetfulness caused by poor liver function
- Reduced levels of platelets, blood cells that help form blood clots, or white blood cells, the cells that fight infection
Diagnosis is made clinically by the presence of ascites, vatical bleeding, splenomegaly, and using imaging techniques such as X ray chest, endoscopy , USG etc.
CASE 2
A 29 year old female patient came to the OPD on a wheel chair with chief complaints of
• left sided chest pain- non radiating, stabbing type since 1 month.
• abdominal distension- gradually progressive since 1 month.
• association with fever during the evenings.
PAST HISTORY:
• First pregnancy( 2016) ended in spontaneous abortion.
• Second pregnancy ( 2017) ended in an intra uterine death.
• Later developed DM for which he was kept on oral hypoglycemic agents
• Third pregnancy ( 2019) was successful.
Had polyhydramnios and DM- used OHA
• After the third delivery, sugar levels came back to normal- stopped OHA
• later ( feb 2020) developed chest pain and abdominal distension ( present complaints ) with evening raise of temp for a week
• pt is a k/c/o Diabetes mellitus - started on tab metformin and tab glimiperide
* before coming to this hospital, the patient went to a local hospital where increased levels of pancreatic amylase and lipase were detected- suspected pancreatitis
EXAMINATION:
Patient conscious coherent cooperative.
VITALS:
• Temp- 98.4 F
• Pulse- 97 bpm
• BP- 100/70 mmhg
• RR- 24 cycles/min
CVS , CNS- normal on examination
RESPIRATORY SYSTEM:
Breath sounds- normal
P/A
• Inspection
Distended. Flanks full
Umbilicus central, everted
Striae present
No dilated veins
•Palpation
Soft
Diffuse tenderness all over
No organomegaly
• Percussion
Shifting dullness present
•Auscultation
Bowel sounds heard
INVESTIGATIONS:
•Hemogram: hb-9.6 g/dl, tlc-6700,pcv-28.6, plt-4.38
•ESR # 80 mm/ 1 st hour
•LFT
Total Bilurubin 0.62 mg/dl
Direct bilirubin # 0.22 mg/dl
SGOT(AST) 20 IU/L
SGPT(ALT) 22 IU/L
Alkaline phosphatase # 232 IU/L
Total protein # 6.0 gm/dl
Albumin # 2.0 gm/dl
A/G RATIO 0.52
•RFT
Urea # 10 mg/dl
CREATININE 0.6 mg/dl
Uric acid # 8.7 mg/dl DHBS
CALCIUM 9.6 mg/dl
PHOSPHOROUS 3.9 mg/dl
SODIUM 139 mEq/L
POTASSIUM 4.0 mEq/L
CHLORIDE 101 mEq/L
• USG REPORT
Mild to moderate ascites- echogenic fluid
Rt kidney- irregular calycial dilation noted
• CHEST X-Ray
Mild to moderate pleural effusion on left side
• Thoracocentasis was done

Pleural fluid analysis: sugar-246mg/dl
protein-6.1gm/dl
Pleural fluid analysis : exudative
• Multiple paracentesis was done with 500 ml draining out each time. - Refractory ascites

Ascitic fluid amylase - 15 - rules out pancreatic ascites
Ascitic fluid protein- 4.1
Sugar- 147
Ascitic fluid LDH- 431
Serology - negative
Ascitic albumin-1.7
Saag-0.5
Ascitic fluid LDH- 431
Serology - negative
Ascitic albumin-1.7
Saag-0.5
•The patient was advised for a DIAGNOSTIC LAPAROSCOPY + PERITONEAL/ OMENTAL BIOPSY
REPORT-
Microscopy sections revealed chronic inflammatory cell infiltrate with fibrocollagenous tissue.
Sections studied shows lobules of mature adipocytes with chronic inflammatory cell infiltrate with lymphocytes, plasma cell, epitheloid cells and few neutrophils and multi nucleated gaint cells.
IMPRESSION:
* Peritoneum - suggestive of chronic peritonitis
* Omentum- suggestive of granulomatous omentitis


PROVISIONAL DIAGNOSIS:
Chronic inflammation of the peritoneum secondary to
• tuberculosis
• immune mediated inflammation of the peritoneum.
TREATMENT:
• patient was put on ATT ( anti tubercular therapy)in view of her diagnosis
• later developed arthritis due to hyerurecemia ( adverse affect of tab pyrazinamide, an AAT ) for which she was put on allopurinol
* WHY WERE PANCREATIC ENZYMES RAISED WITH NO EVIDENCE OF PANCREATIC INVOLVEMENT???
“Serum lipase and amylase activity levels are used traditionally in the diagnosis of pancreatitis. However, in recent years, many investigators have demonstrated the production of pancreatic enzymes in infectious diseases that do not necessarily involve the pancreas.
Lipase and amylase activity levels are elevated mildly in patients with TB. The cause of this elevation is not known. Lipase enzyme activity levels appeared to increase with increasing ESR, a marker of inflammation, which in turn diminished with duration of treatment, which suggests a possible effect of mycobacteria on lipase levels. Although amylase enzyme levels were elevated in patients, there was no correlation with any of the parameters measured and no explanation could be found for this phenomenon, thus the role of amylase in TB remains enigmatic.”


Comments
Post a Comment